January 16, 2026
Hip bursitis is often described as a localized problem—inflammation in the hip that needs rest, ice, or injections. Yet at my Downtown Toronto clinic, I regularly meet patients who have tried exactly that, only to find their hip pain keeps returning.
Whether it’s professionals spending long hours seated near Bay Street or active Torontonians walking, running, or cycling along the Don Valley Trail, hip bursitis is rarely just a hip problem. In many cases, it is the end result of low back dysfunction and glute inactivation, which places excess mechanical stress on the hip and leads to irritation and inflammation over time.
In this article, we’ll break down what hip bursitis really is, the different types of hip bursitis, and why managing the hip in isolation often falls short. More importantly, we’ll explore how corrective chiropractic care can help by addressing the root cause—not just the inflamed tissue.
What Is Hip Bursitis?
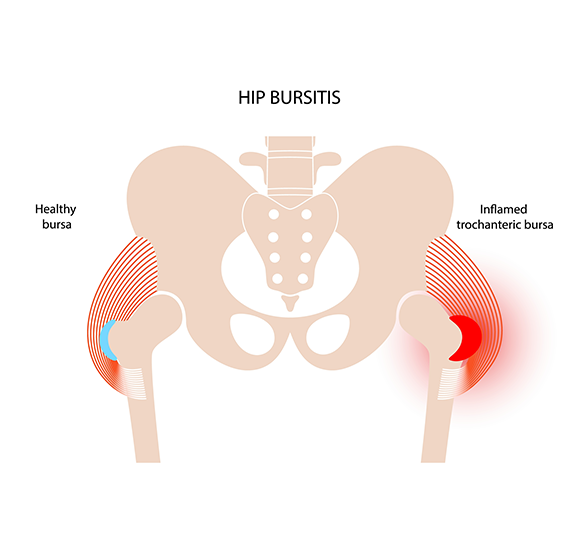
A bursa is a small, fluid-filled sac that reduces friction between muscles, tendons, and bones. The hip contains several bursae designed to help the joint move smoothly during walking, standing, and rotation.
Hip bursitis occurs when one or more of these bursae become irritated or inflamed, leading to pain, tenderness, and movement discomfort.
Common symptoms include:
While inflammation is part of the picture, it’s important to understand that bursae usually become irritated because of abnormal load or movement, not spontaneously.
Types of Hip Bursitis
1. Trochanteric Bursitis
This is the most commonly diagnosed form of hip bursitis. It involves inflammation of the bursa over the greater trochanter, the bony prominence on the outside of the hip.
Symptoms often overlap with what is now referred to as Greater Trochanteric Pain Syndrome, including lateral hip pain and tenderness. Research suggests that this condition frequently coexists with gluteal tendon dysfunction, rather than isolated bursal inflammation (PubMed).
2. Iliopsoas (Anterior Hip) Bursitis
This type affects the bursa at the front of the hip, near the iliopsoas muscle. It may cause groin or anterior hip pain and discomfort during hip flexion or walking uphill.
Iliopsoas bursitis is often associated with altered pelvic mechanics, prolonged sitting, or compensatory movement patterns originating from the lower back.
3. Ischial Bursitis
Less common, ischial bursitis affects the bursa near the ischial tuberosity—the “sitting bone.” Pain is typically felt when sitting on hard surfaces or during activities involving hip extension.
Although the location differs, the underlying issue is often the same: abnormal load due to poor neuromuscular control.
Why Treating the Hip Alone Often Fails
The Inflammation Trap
Conventional management of hip bursitis often focuses on reducing inflammation through rest, ice, anti-inflammatory medications, or injections. While these strategies may provide short-term relief, they often fail to address why the bursa became irritated in the first place.
The Canadian Chiropractic Association emphasizes that musculoskeletal pain frequently stems from joint dysfunction and altered movement patterns, not just local tissue irritation (Canadian Chiropractic Association).
When the underlying mechanics remain unchanged:
This is why many patients feel better temporarily, only to experience flare-ups weeks or months later.
The Real Issue: Low Back Dysfunction and Glute Inactivation
How the Lower Back Drives Hip Stress
The hip does not function independently—it is part of a kinetic chain involving the spine, pelvis, and lower limbs. Proper hip stability relies heavily on glute muscle activation, which is controlled by nerve signals originating in the lumbar spine.
When the lower back is stiff, restricted, or misaligned:
The Ontario Chiropractic Association highlights that spine health and posture are critical for maintaining efficient muscle function and joint loading (Ontario Chiropractic Association).
Glute Inactivation and Excess Hip Load
When the glutes fail to do their job, other tissues around the hip—including bursae—are forced to absorb forces they were never designed to handle. Over time, this increased mechanical stress can lead to irritation, inflammation, and pain.
In other words, the bursa becomes inflamed not because it is weak or damaged—but because it is overworked.
Expert Insight: Dr. Mateusz Krekora’s Perspective
At Dr. Mateusz Krekora Chiropractic Clinic, I often explain to patients that hip bursitis is usually a symptom, not the root problem.
Clinically, many individuals with recurring hip bursitis also demonstrate:
If care focuses only on the hip, the underlying stress pattern remains. That’s why a corrective, NeuroStructural approach is essential for long-term improvement and relief.
How Corrective Chiropractic Care Helps Hip Bursitis
Addressing Low Back Dysfunction
Corrective chiropractic care focuses on restoring proper spinal motion, alignment, and nervous system function—particularly in the lower back and pelvis.
Chiropractic care is recognized by the Government of Canada as a regulated profession focused on neuromusculoskeletal health (Government of Canada).
By improving spinal function:
This decreases the mechanical stress that contributes to bursal irritation.
Re-Activating the Glutes
Once spinal communication improves, corrective care aims to support proper glute activation, allowing these muscles to resume their role as primary stabilizers of the hip.
As the glutes take on their intended workload, the bursae are no longer forced to compensate—giving inflammation a chance to resolve naturally.
Supporting Recovery with Electroacupuncture
In some cases, electroacupuncture is used alongside chiropractic adjustments to support neuromuscular function and pain modulation.
While research is ongoing, current evidence suggests electroacupuncture may help:
Peer-reviewed studies indexed on PubMed indicate electroacupuncture can be beneficial for chronic musculoskeletal pain conditions (PubMed).
When used appropriately, electroacupuncture can help calm irritated tissues while reinforcing proper muscle engagement—supporting the corrective process.
Local Tips for Managing Hip Bursitis in Toronto
To reduce unnecessary stress on the hip while undergoing care:
These strategies are most effective when combined with professional care that addresses spinal and neuromuscular health.
Conclusion
Hip bursitis is often mismanaged by treating the hip in isolation, without addressing the underlying causes of excess load and stress. In many cases, low back dysfunction and glute inactivation are the true drivers of recurring inflammation.
Corrective chiropractic care focuses on restoring spinal function, reactivating the glutes, and reducing abnormal hip stress—helping patients move better and feel stronger over time.
At Dr. Mateusz Krekora Chiropractic Clinic, our NeuroStructural approach is designed to correct the root cause, not just manage symptoms.
👉 Book Your Free Case Review today and start feeling like you’re 25 again.
This article is for informational purposes only and should not be taken as medical advice. Please consult a licensed chiropractor before starting any treatment.
