February 6, 2026
Introduction
If you’ve been told you have medial meniscus pain, chances are your journey has looked something like this: months of physiotherapy, endless glute and quad exercises, temporary relief at best—and persistent knee pain at worst. Eventually, an MRI shows mild meniscus damage, and suddenly surgery is on the table.
At my Toronto clinic, I often meet patients at this exact crossroads. They’re active, disciplined, and frustrated. They’ve “done everything right,” yet their knee still hurts—especially walking downstairs, squatting, or getting up after sitting at a desk all day on Bay Street.
What’s often missed in medial meniscus pain isn’t effort or compliance.
It’s looking up the chain.
Understanding Medial Meniscus Pain
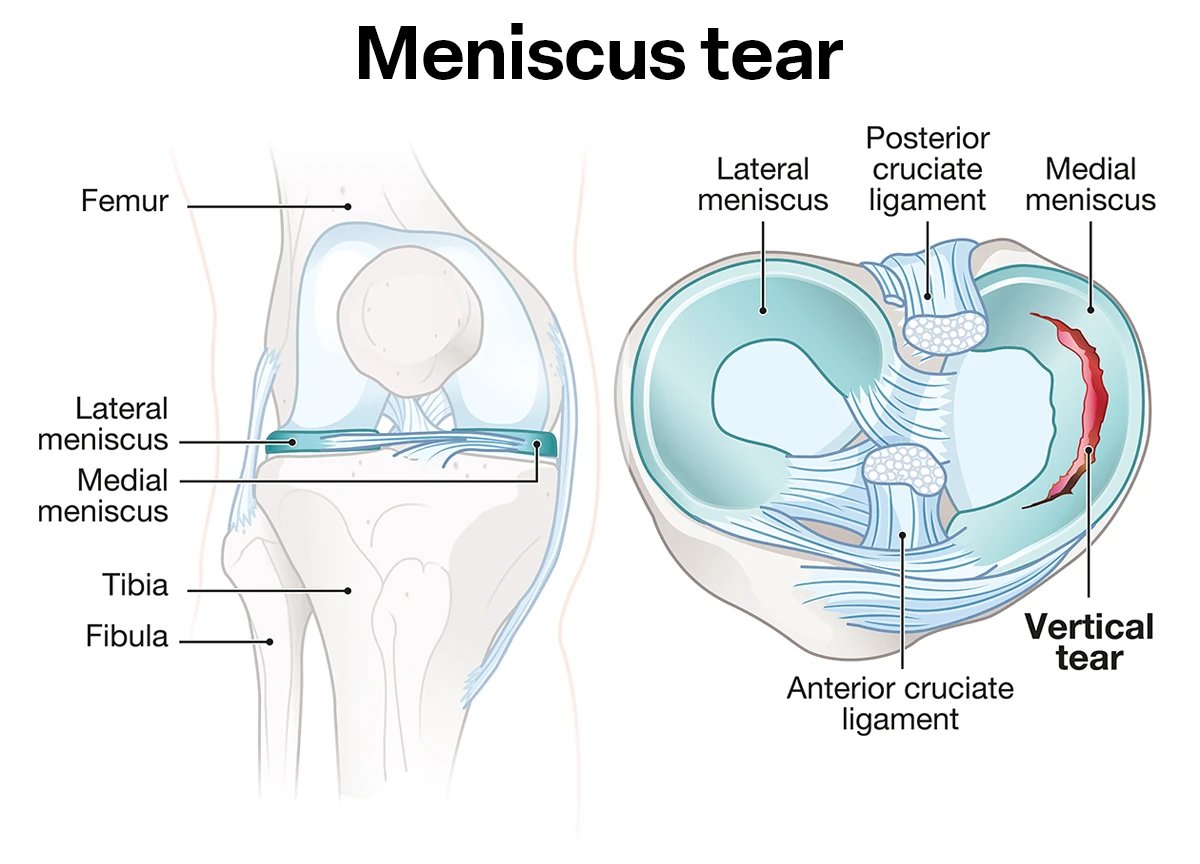
The medial meniscus is a C-shaped piece of cartilage on the inner side of your knee. Its job is to absorb shock, stabilize the joint, and distribute load during movement like walking, running, or cycling the Don Valley Trail.
Meniscus-related pain is commonly associated with:
MRI findings often show mild or degenerative meniscal changes, especially in adults over 30. Importantly, research shows that meniscal changes on MRI are extremely common—even in people without knee pain (Government of Canada – Musculoskeletal Health).
Yet once that MRI report comes back, the clinical focus often narrows dramatically to the knee itself.
The Typical (and Incomplete) Approach
1. Strengthen the Glutes and Quads
Physiotherapy programs for medial meniscus pain usually emphasize:
These are not wrong. In fact, they’re often necessary.
But here’s the critical question I ask patients at Dr. Mateusz Krekora Chiropractic Clinic:
“Are you actually able to use the strength you’ve built?”
2. Persistent Pain Despite “Doing the Work”
Many patients come to me saying:
This is where conventional care often hits a wall.
The MRI → Surgery Pipeline
After months of persistent pain:
However, large reviews published in peer-reviewed journals have shown that arthroscopic surgery for degenerative meniscus issues often performs no better than conservative care in many cases (PubMed – Meniscal Surgery Outcomes).
So why are people still in pain?
Because the meniscus may not be the primary driver.
Expert Insight: What I See as a Corrective Chiropractor
As a NeuroStructural Corrective Care chiropractor, I approach medial meniscus pain differently.
At my Toronto clinic, I often see that no one has thoroughly assessed:
Strength Without Activation Is Useless
You can have:
…but if your nervous system isn’t properly activating those muscles during walking, squatting, or load transfer, your knee will continue to take excessive stress.
This concept aligns with the neurological principles recognized by the Canadian Chiropractic Association, which highlights the role of spinal health in movement and neuromuscular coordination (Canadian Chiropractic Association).
Looking Up the Chain: Why the Spine Matters
The knee does not operate in isolation.
The Kinetic Chain Problem
When spinal segments—particularly in the lumbar spine and pelvis—lose proper alignment or motion:
Over time, this altered movement pattern increases stress on the medial meniscus.
This is why simply strengthening muscles without correcting spinal and neurological dysfunction often fails.
NeuroStructural Examination: What’s Different
When patients with medial meniscus pain undergo a NeuroStructural examination, we assess:
This type of examination goes beyond symptom location and looks for root causes, a core principle supported by the Ontario Chiropractic Association’s emphasis on functional, evidence-informed care (Ontario Chiropractic Association).
How NeuroStructural Corrective Care Helps
Once the underlying issues are identified, care focuses on:
When this happens, patients often report:
Importantly, this approach does not replace rehab exercises—it complements it by ensuring the body can actually use the strength being built.
Local Tips for Supporting Knee Recovery in Toronto
While corrective care addresses the root cause, daily habits matter too:
At my clinic, I help patients integrate corrective care with realistic lifestyle adjustments that fit Toronto living.
Conclusion: Don’t Stop at the Knee
Medial meniscus pain is rarely just about cartilage damage.
If you’ve:
…it may be time to ask a different question:
Is my nervous system actually coordinating my movement the way it should?
Is your spine contributing to your persistent knee pain?
At Dr. Mateusz Krekora Chiropractic Clinic, our NeuroStructural approach focuses on restoring function from the spine outward—so your body can finally use the strength you’ve worked so hard to build.
👉 Book Your Free Case Review and take the next step toward lasting knee relief.
